AI-Driven Healthcare Automation: The Engine Behind Hyperautomation

Today, the healthcare space is standing at a breaking point more than ever. Hospitals worldwide are overwhelmed with rising patient volumes, administrative overload is consuming more clinician time than care itself, and data is multiplying faster than teams can process it. The industry’s most crucial resource, its workforce, is stretched thin, while the demand for accuracy, speed, and affordability continues to intensify. In the middle of this pressure, is emerging as the most practical and scalable solution: AI-driven healthcare automation.
This shift goes far beyond traditional task-level automation. It’s the beginning of a new operating model where artificial intelligence, intelligent workflows, and hyperautomation converge to eliminate inefficiencies, accelerate decision-making, and fundamentally redesign how care is delivered.
We’re no longer debating whether automation belongs in healthcare; we’ve already crossed that threshold. The real challenge now is how rapidly organizations can scale AI-driven healthcare automation to stay resilient, responsive, and future-ready in a system that demands nothing less.
What AI-Driven Healthcare Automation Really Means for Today’s Healthcare Systems
Hyperautomation has moved from a future vision to a present-day operational necessity. In today’s hospitals and health systems, it represents a powerful fusion of advanced technologies designed to automate not just tasks, but entire end-to-end workflows. Unlike traditional automation, which focused on isolated, rule-based steps, hyperautomation builds a connected, intelligent ecosystem where data flows seamlessly, decisions are AI-augmented, and processes continuously optimize themselves.
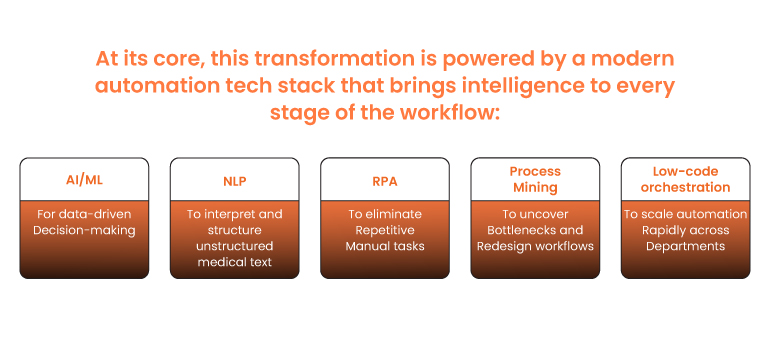
At its core, this transformation is powered by a modern automation tech stack that brings intelligence to every stage of the workflow:
For a deeper dive into how this shift began, you can revisit our October Tech Newsletter on Hyperautomation.
Why Healthcare Needs Hyperautomation Now More Than Ever
Healthcare isn’t just complex, it’s chronically overburdened. Administrative workload continues to rise, clinicians spend nearly half their day managing documentation, and revenue cycle teams face growing claim denials and compliance demands. At the same time, patient expectations for speed, transparency, and personalized care have never been higher.
Hyperautomation powered by AI-driven healthcare automation meets this moment by targeting the root inefficiencies that drain capacity, slow decisions, and inflate costs. It enables hospitals to streamline high-friction workflows, unlock real-time insights, and free clinical teams to focus on what matters most: delivering quality care.
High-Impact Use Cases Transforming Healthcare
The impact of AI-driven healthcare automation becomes most evident when we look at how it is reshaping everyday workflows across hospitals and health systems. From patient-facing interactions to back-office financial operations to clinical decision support, hyperautomation is enabling faster processes, higher accuracy, and more intelligent resource utilization. Below are three of the most widely adopted and high-value use cases gaining momentum across the industry today.
Patient Onboarding & Intake
Patiet intake has long been plagued by delays, repetitive paperwork, and data entry errors. Through AI-powered intelligent document processing, health systems can automatically extract information from forms, insurance cards, and prescriptions with high accuracy.
NLP-driven virtual assistants support patients with scheduling, pre-visit instructions, and ongoing queries. Together, these capabilities reduce administrative burden, shorten wait times, and integrate seamlessly with EHR systems, creating a smoother, more predictable patient journey.
Revenue Cycle & Claims Automation
Revenue cycle operations are under pressure from rising claim denials, labor shortages, and strict compliance requirements. AI-augmented RPA automates repetitive tasks like eligibility checks and claim submissions, while machine-learning models identify missing fields, detect anomalies, and forecast denial risks before they occur.
Organizations adopting this approach are seeing faster reimbursements, reduced leakage, and improved audit readiness, strengthening financial stability without adding headcount.
Clinical & Operational Workflow Automation
Beyond administration, hyperautomation is now transforming core clinical and operational processes. AI-driven systems generate clinical summaries, automate documentation, and power smarter triage recommendations. Operationally, predictive analytics enables intelligent staff scheduling based on patient-volume forecasts, reducing burnout risks and improving throughput.
These capabilities help clinicians reclaim time from paperwork, accelerate decision-making, and deliver care with greater consistency and efficiency.
How to Implement Hyperautomation: Step-by-Step
- Discover and Map
Run process mining and workflow analysis to identify high-friction areas and quantify time/cost savings. - Prioritise Quick Wins
Select 2–3 pilot workflows with clear ROI (claims processing, patient intake, documentation). - Design the Automation
Define end-to-end flows, data contracts, and integration points with EHRs and core systems. - Build Intelligence
Integrate AI models NLP for text, IDP for forms, anomaly detection for finance, and validate on real data. - Deploy aPlatform
Use a low-code orchestration hub to deploy bots, schedule jobs, and centralise logging. - Govern and Monitor
Implement access controls, model monitoring, automated audits, and human-in-loop checkpoints. - Scale with Feedback
Use ML insights and performance metrics to expand automation into adjacent processes iteratively.
Challenges and Governance Essentials
Implementing hyperautomation in healthcare comes with real challenges, including legacy systems, fragmented data, strict compliance requirements, and the need for strong change management. AI introduces additional concerns such as bias, explainability, and patient safety, which must be addressed thoughtfully.
Healthcare organizations should always maintain a human-in-the-loop approach for clinical decisions. Strong governance is essential, supported by automated audits, rigorous access control, and continuous model monitoring to ensure accuracy, transparency, and trust.
The Future: Autonomous Healthcare Operations
The next decade is expected to accelerate the shift toward autonomous operations, driven by the rapid evolution of AI-driven healthcare automation. Intelligent agents will manage end-to-end workflows, coordinating everything from intake to discharge with minimal manual intervention. Digital twins will provide real-time operational insights, predicting bottlenecks and guiding resource allocation.
As these capabilities mature, hospitals will function as self-optimizing systems where processes continually adjust based on demand and clinical needs. Patients will experience personalized, automated care pathways that anticipate their requirements and deliver support proactively.
Wrapping Up
Hyperautomation combined with AI has emerged as one of the most powerful forces reshaping modern healthcare, enabling organizations to move faster, operate smarter, and deliver more consistent outcomes. As the pressure on health systems intensifies, AI-driven healthcare automation is no longer optional; it is the foundation for resilience and long-term transformation. Healthcare leaders must begin by strengthening their data foundations, identifying automation-ready workflows, and building scalable, intelligent operations that can evolve with changing demands.
Neutrino enables this shift through deep industry research, proven automation frameworks, and enterprise-grade solutions. Our AI-powered intelligent document processing platform, NimbleDox, helps healthcare organizations streamline documentation, eliminate bottlenecks, and accelerate hyperautomation at scale. With the right strategy and the right partners, the future of autonomous, patient-first healthcare is within reach.
