AI-Powered Prior Authorization: Reducing Burnout, Restoring Focus on Patients

Prior authorization was designed to ensure appropriate, cost-effective care, but in reality, it has become one of the biggest pain points in healthcare delivery. With the rise of AI-Powered Prior Authorization, there is now a growing push to address these long-standing inefficiencies. The process is still largely manual, requiring endless forms, phone calls, and back-and-forth between payers and providers.
According to the American Medical Association, 94% of physicians say prior authorization leads to delays in necessary treatment. These delays don’t just frustrate clinicians but increase administrative burden, contribute to burnout, and leave patients waiting for critical care. This is why AI-Powered Prior Authorization is emerging as a transformative solution. By bringing intelligence, automation, and compliance together, it offers a way to streamline approvals, reduce friction for care teams, and put the focus back where it belongs, i.e., on patients.
The Traditional Challenge Before AI-Powered Prior Authorization
Traditional prior authorization remains one of the most frustrating hurdles in healthcare. The process is dominated by manual reviews, repetitive phone calls, and outdated fax-based exchanges that slow down critical decisions. A major barrier is the lack of interoperability between payers and providers, which fuels inefficiencies and miscommunication.
The result is a heavy administrative burden that leaves clinicians drained and patients waiting. In fact, the American Medical Association reports that these delays often compromise timely care, underscoring the urgent need for solutions that simplify and modernize the system.
Tangible Benefits for Healthcare Stakeholders
AI-Powered Prior Authorization is delivering measurable improvements across the healthcare ecosystem.
- For providers, it eases the administrative load and shortens turnaround times, freeing resources for higher-value work.
- Clinicians gain more time with their patients, reducing burnout and improving the quality of interactions.
- Payers and managed care organizations benefit from streamlined processes that enhance efficiency, lower operational costs, and help curb fraud.
- Most importantly, patients experience quicker access to the treatments they need, greater satisfaction, and improved health outcomes.
A recent study found that automation in prior authorization can save the industry billions annually, highlighting the potential for AI-driven solutions to create a lasting impact.
Neutrino’s Approach to AI-Powered Prior Authorization
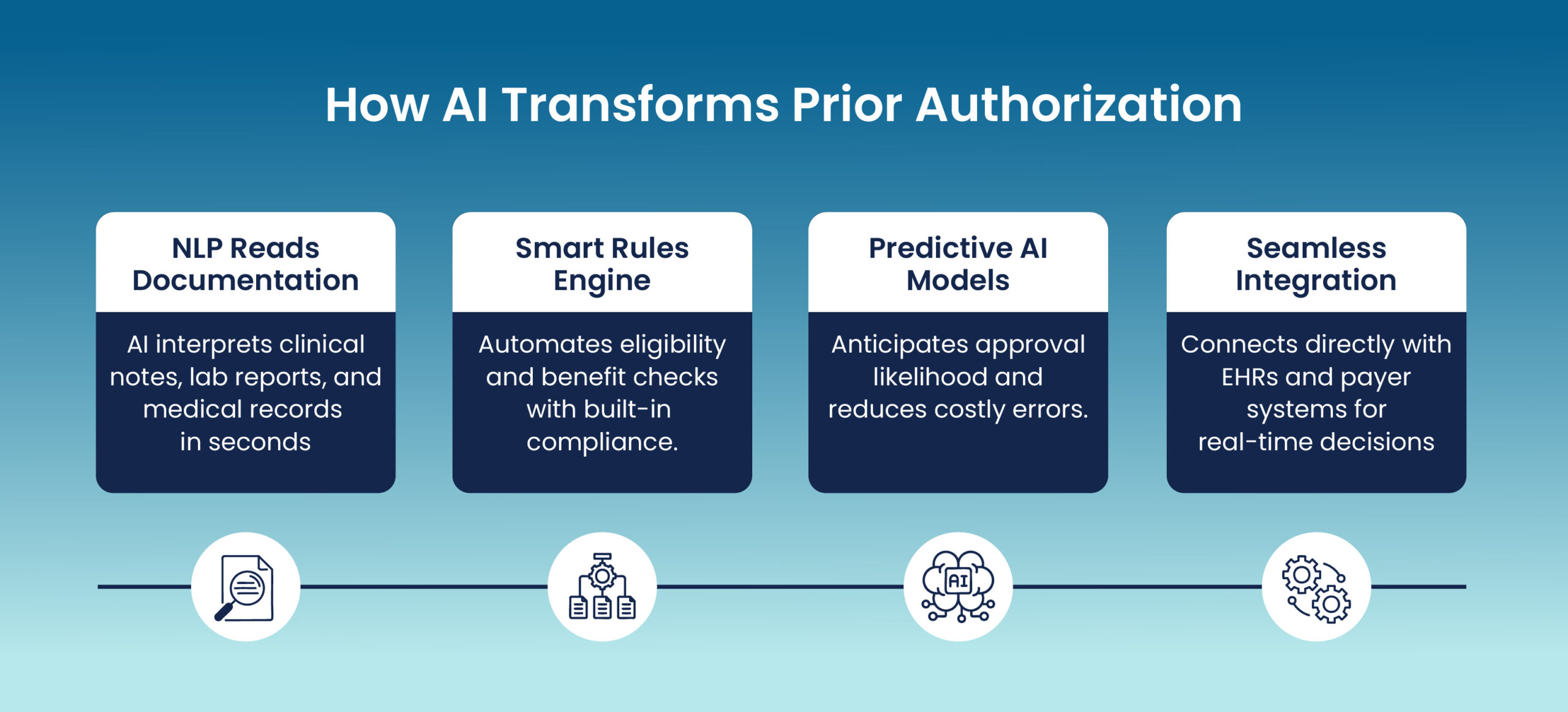
Our approach to AI-Powered Prior Authorization focuses on making healthcare processes smarter, faster, and more patient-centric. Our AI voice bots handle benefit verification calls, reducing administrative burdens on staff while ensuring patients receive timely information.
Agentic AI systems manage multi-step approvals in real time, adapting to complex workflows seamlessly. Built on a cloud-native infrastructure, our solutions scale securely and integrate effortlessly across payers and providers.
With MLOps tailored for healthcare, continuous monitoring and compliance are embedded at every stage. A hyperautomation layer combines AI, RPA, and APIs to deliver end-to-end automation, helping healthcare teams focus on what truly matters: enhancing care and improving patient experiences.
Real-World Impact & Use Cases
AI-Powered Prior Authorization is driving meaningful improvements across healthcare:
- Oncology treatments: Accelerates approvals so patients can begin critical therapies without delay.
- High-volume medication requests: Automates routine submissions, reducing manual intervention for care teams.
- Recurring approvals: Handles repetitive requests in minutes, saving valuable clinical time.
- Efficiency for payers and providers: Generates significant time and cost savings.
According to a recent study, automation in prior authorization could save the U.S. healthcare system over $400 million annually.
What the Future Holds: From Automation to Intelligent Collaboration
The future of prior authorization is moving rapidly from basic automation to intelligent collaboration between payers, providers, and patients. AI-Powered Prior Authorization will evolve beyond task automation into adaptive, agentic systems capable of learning and responding in real time.
This shift opens the door to greater alignment with value-based care models, ensuring that approvals not only reduce delays but also support better outcomes and cost efficiency. Regulatory frameworks are also beginning to adapt, creating opportunities for more scalable innovation.
A recent McKinsey report estimates that AI-driven automation could free up to 20 percent of healthcare staff time, underscoring the potential for smarter systems to transform care delivery at scale.
Wrapping Up
AI-Powered Prior Authorization is not just a tool but a meaningful shift toward smarter, faster, and more responsible healthcare. By streamlining processes, reducing administrative friction, and creating space for clinicians to focus on care, it is helping reshape how healthcare organizations operate.
This transformation goes beyond efficiency it is about enabling better outcomes and restoring balance between technology and the human side of medicine. At Neutrino, we are building AI-first healthcare solutions that bring intelligence, automation, and responsibility together. Our goal is to help organizations modernize prior authorization while ensuring patients remain at the center of care. Discover how we can support your journey toward more intelligent and human-centered healthcare.
