Elevating Patient Adherence: A Strategic Imperative in Modern Healthcare

- July 10, 2025
Even the best healthcare fails when a patient discontinues treatment midway. As per the WHO, despite advances in access and affordability, nearly 50% of patients with chronic conditions don’t adhere to their prescribed medications and therapies. The consequences ripple across the system, including worsening health, preventable hospitalizations, and an estimated $500 billion in annual global healthcare costs tied to non-adherence, according to a report.
The problem isn’t just forgetfulness; there are various factors, including fatigue, fear, complexity, and a lack of support, that truly fit patients’ lives. Patient reminders and apps often fall short, either too generic, poorly timed, or unreliable when it matters most. For too long, adherence programs have focused on compliance instead of understanding.
That’s changing. A new approach is emerging, one that centers on the patient as a whole person, not just a recipient of reminders. As the World Economic Forum notes, the future of healthcare lies in empathetic, AI-enabled, patient-first ecosystems that personalize engagement and rebuild trust.
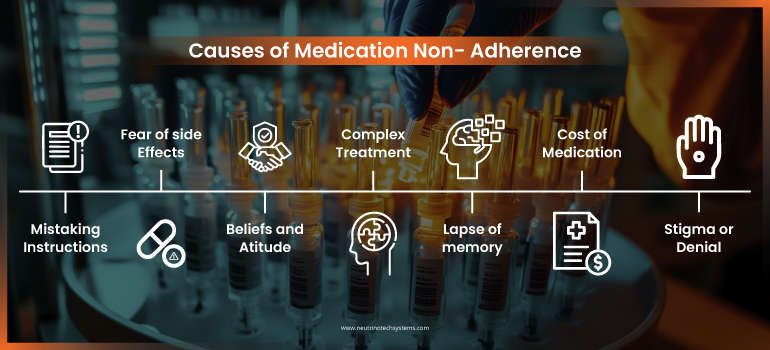
Why Patients Struggle to Adhere
Adherence is shaped by real-life challenges, side effects, confusing instructions, demanding schedules, or emotional fatigue. Psychological barriers like fear, denial, and uncertainty can be just as limiting as physical ones. Addressing patient adherence in the US means understanding these layers, not just prescribing solutions.
Then come the practical challenges that often go unaddressed in medication adherence strategies, such as:
- Complex medication regimens that are difficult to follow
- High out-of-pocket costs are making treatment financially unsustainable
- Transportation issues that limit access to pharmacies or clinics
Each of these adds friction to a patient’s ability to stay on track, yet they’re often overlooked in support design.
Many patient adherence programs miss the mark because they don’t fit into the realities of patients’ daily lives. It’s not just about more instructions, it’s about care that feels relevant and manageable.
There is often a gap between what healthcare providers communicate and what patients actually understand. These disconnects can lead to confusion, mistrust, or hesitation, making adherence not just a clinical issue but a deeply human one.
Evolving Patient Support: From Automation to Empathy
While technology has significantly accelerated patient support in the last two decades, it has not always preserved the human element that patients value. Traditional processes focused on logistics such as delivering medications, managing approvals, and sending reminders. These were essential, but often one-size-fits-all. Today’s tech-enabled hub services have taken a leap forward, offering more coordinated support across access, affordability, and engagement.
But the real shift lies in moving from automation to empathy. Today, Generative AI is becoming a powerful tool in this evolution, enabling 24/7, responsive interactions that adapt to a patient’s needs and real-world behavior. It can simplify treatment plans, anticipate support gaps, and provide timely guidance that feels intuitive and relevant.
In practice, GenAI is already helping healthcare providers reduce waiting times and streamline care coordination, making support more immediate and aligned with each patient’s journey.
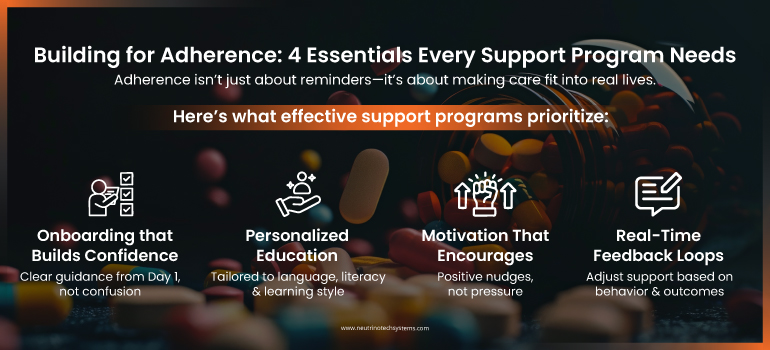
Designing Adherence-Focused Support Programs
Patient adherence in the US is a continuous process that requires structure, consistent guidance, and adaptable support at every stage of the patient journey. It’s not static, it evolves with the patient’s needs, circumstances, and understanding over time.
To truly support patients, programs must be designed for real-life behavior, not ideal scenarios. The most effective ones focus on:
- Clear onboarding that builds confidence from day one
- Ongoing education tailored to a patient’s literacy, language, and learning style
- Consistent motivation, through encouragement, not enforcement
- Real-time feedback loops that help patients and care teams adjust together
The Role of GenAI in Strengthening Patient Adherence
As patients’ requirements become more complicated globally, the capacity to provide timely, individualized support becomes increasingly important. Studies show that when communication is simplified and tailored to patient comprehension, adherence significantly improves. This underscores GenAI’s potential to clarify instructions and align messaging with individual needs.
GenAI offers constant conversational engagement that adapts to a patient’s needs and behavior. It can make treatment instructions easier to understand, answer common inquiries, and provide nudges that feel natural rather than clinical. For patients managing chronic diseases or multi-drug regimens, this degree of tailored, on-demand support can make adherence more manageable and less daunting.
When thoughtfully integrated, GenAI supports, not sidelines, care teams. It frees up staff for high-touch interventions while handling routine interactions with consistency and empathy.
In a world where reminders alone are no longer enough, GenAI helps shift adherence from a passive task to an active, supported experience at scale, in context, and on the patient’s terms.
The Path Forward
Strengthening adherence begins at the design stage, not as a reaction to missed doses, but as a proactive strategy built into every touchpoint of the care journey.
True personalization goes beyond digital dashboards; it must reflect how people think, feel, and live. GenAI and other technologies can elevate this experience, but they are enablers, not replacements, for human connection. The most effective programs are those that are anticipatory, responsive, and deeply aligned with the realities of patient behavior.
Although healthcare has no shortage of technologies, non-adherence remains a persistent challenge, not from a lack of tools, but from a gap in connection. At Neutrino Tech Systems, we’ve partnered with leading global healthcare organizations to bridge that gap, designing support ecosystems that combine intelligent triage, personalized engagement, and behavior-aware workflows.
Our solutions integrate seamlessly with EHRs and patient access platforms to make care not just accessible, but truly supportive, adapting to how patients live, decide, and heal.
